American Heart Association Renders Itself Obsolete With 1960s Dietary Advice on Coconut Oil
More Information
By Dr. Mercola
For well over half a century, a majority of health care officials and media have warned that saturated fats are bad for your health and lead to obesity, high cholesterol and heart disease. The American Heart Association (AHA) began encouraging Americans to limit dietary fat in general and saturated fats in particular as far back as 1961.
The current version of the U.S. Department of Agriculture’s (USDA) food pyramid, called “MyPlate,”1 more or less eliminated fats altogether, with the exception of a small amount of low-fat dairy. According to MyPlate, the food groups are fruits, vegetables, grains, protein and dairy — not the three biological building blocks known as carbohydrates (fruits, veg, grains), protein and fats.
All the while, studies have repeatedly refuted the wisdom of these low- to no-fat recommendations. Now all of a sudden, the AHA is coming out with warnings reminiscent of the 1960s all over again.
If you’ve followed the news lately, you will have seen bold headlines declaring coconut oil dangerous, and that you should switch from butter to margarine to protect your heart health! How is this even possible? It’s akin to the flat Earth theory that inexplicably gained traction in the 21st century despite clear and indisputable proof that we indeed live on a planetary sphere.
Many have expressed confusion and bewilderment in response to the AHA’s margarine push, and no wonder. Let’s not forget that creating doubt is a core strategy used by industry to delay change. This margarine-promotion also happens to conveniently sync up with news about a vaccine to lower cholesterol2,3 — a strategy that would be unnecessary if people were to just eat healthy saturated fats like coconut oil and butter, and eliminate processed foods and sugar.
AHA Sends Out Warning to Cardiologists Around the World
According to the AHA’s latest advisory,4 saturated fats such as butter and coconut oil should be avoided to cut your risk of heart disease. Replacing these fats with polyunsaturated fats such as margarine and vegetable oil might cut heart disease risk by as much as 30 percent, about the same as statins, the AHA claims.
This Presidential Advisory was sent out to cardiologists around the world, not just to those in the U.S. Overall, the AHA recommends limiting your daily saturated fat intake to 6 percent of daily calories or less.5 According to The Daily Mail:6
“The scientists analyzed all available evidence on the subject and found saturated fat — such as that found in butter, whole milk, cream, palm oil, coconut oil, beef and pork — was linked to an increased risk of heart disease.
Replacing this with polyunsaturated fat — found in spreads and vegetable oils — or monounsaturated oils found in olive oil, avocados and nuts — cuts the risk of heart problems. The study … bolsters NHS advice that saturated fat should be lowered in the diet.
Lead author professor Frank Sacks, of Harvard School of Public Health, said: ‘We want to set the record straight on why well-conducted scientific research overwhelmingly supports limiting saturated fat in the diet to prevent diseases of the heart and blood vessels. Saturated fat increases LDL — bad cholesterol — which is a major cause of artery-clogging plaque and cardiovascular disease’ …
The authors, however, warned that not all margarines and spreads are healthy. They found that some forms of margarine which use ‘trans fats’ — a type of fat which improves shelf life — actually raise the risk of heart disease.”
Victoria Taylor, senior dietician at the British Heart Foundation, also made sure to note that “lifestyle change should go hand in hand with taking any medication prescribed by your doctor; it shouldn’t be seen as one or the other.” In other words, don’t think you can avoid statins simply by eating right.
USA Today announced the AHA’s advisory with the nonsensical headline “Coconut Oil Is About as Healthy as Beef Fat or Butter.”7 Why, yes, it is! But here they’re trying to say that all of these are unhealthy, which is altogether backward and upside-down. According to the AHA:
“Because coconut oil increases LDL cholesterol, a cause of CVD [cardiovascular disease], and has no known offsetting favorable effects, we advise against the use of coconut oil.”
On What Evidence Does AHA Base Their Recommendation?
How did the AHA come to the conclusion that they were right about saturated fat 60 years ago and have been right all along? In short, by cherry-picking the data that supported their outdated view. As noted by American science writer Gary Taubes in his extensive rebuttal to the AHA’s advisory:8
“The history of science is littered with failed hypotheses based on selective interpretation of the evidence … Today’s Presidential Advisory … may be the most egregious example of Bing Crosby epidemiology [‘accentuate the positive and eliminate the negative’] that I’ve ever seen … [T]hey methodically eliminate the negative and accentuate the positive until they can make the case that they are surely, clearly and unequivocally right …
[T] he AHA concludes that only four clinical trials have ever been done with sufficiently reliable methodology to allow them to assess the value of replacing SFAs with PUFAs (in practice replacing animal fats [with] vegetable oils) and concludes that this replacement will reduce heart attacks by 30 percent …
These four trials are the ones that are left after the AHA experts have systematically picked through the others and found reasons to reject all that didn’t find such a large positive effect, including a significant number that happened to suggest the opposite …
They do this for every trial but the four, including among the rejections the largest trials ever done: the Minnesota Coronary Survey, the Sydney Heart Study and, most notably, the Women’s Health Initiative, which was the single largest and most expensive clinical trial ever done. All of these resulted in evidence that refuted the hypothesis. All are rejected from the analysis.”
Taubes, an investigative science and health journalist who has written three books on obesity and diet, points out that this latest advisory document actually reveals the AHA’s longstanding prejudice and the method by which it reaches its conclusions.
In 2013, the AHA released a report9 claiming “the strongest possible evidence” supported the recommendation to replace saturated fat with polyunsaturated fats (PUFAs). This, despite the fact that several meta-analyses, produced by independent researchers, concluded the evidence for restricting saturated fats was weak or lacking.
The latest advisory document reveals how the AHA could conclude they had the “strongest possible evidence.” Then, as now, they methodically came up with justifications to simply exclude the contrary evidence. All that was left — then and now — were a small number of studies that support their preconceived view of what they think the truth should be.
Studies Included in AHA’s Advisory Are Based on Outdated Science
Would it surprise you to find out that the four studies that made the cut all date from the 1960s and early 1970s? It makes sense, doesn’t it, since those are the eras when the low-fat myth was born and grew to take hold. The problem is, nutritional science has made significant strides since then.
As noted by Taubes, one of the studies included was the Oslo Diet-Heart Study,10 published in 1970, in which 412 patients who’d had a heart attack or were at high risk of heart disease were randomized into two groups: One group got a low-saturated fat, high-PUFA diet along with ongoing, long-term “instruction and supervision” while the other group ate whatever they wanted and received no nutritional counseling whatsoever.
“This is technically called performance bias and it’s the equivalent of doing an unblinded drug trial without a placebo. It is literally an uncontrolled trial, despite the randomization. (… [A]ll the physicians involved also knew whether their patients were assigned to the intervention group or the control, which makes investigator bias all that much more likely.)
We would never accept such a trial as a valid test of a drug. Why do it for diet? Well, maybe because it can be used to support our preconceptions,” Taubes writes.
Taubes goes on to state that he was so curious about this Oslo study he bought a monograph published by the original author. In it, the author describes in more detail how he went about conducting his trial. Interestingly, this monograph reveals that the sugar consumption in the treatment group was only about 50 grams a day — an amount Taubes estimates may be about half the per capita consumption in Norway at that time, based on extrapolated data.11
“In this trial, the variable that’s supposed to be different is the [saturated fat]/PUFA ratio, but the performance bias introduces another one. One group gets continuous counseling to eat healthy, one group doesn’t. Now how can that continuous counseling influence health status?
One way is that apparently, the group that got it decided to eat a hell of lot less sugar. This unintended consequence now gives another possible explanation for why these folks had so many fewer heart attacks. I don’t know if this is true. The point is neither did Leren. And neither do our AHA authorities,” Taubes writes. “All of the four studies used to support the 30 percent number had significant flaws, often this very same performance bias. Reason to reject them.”
Dangerous Advice
Dr. Cate Shanahan,12 a family physician and author of “Deep Nutrition: Why Your Genes Need Traditional Food,” emailed me an even stronger rebuttal, saying “This message from the AHA is not only false, it is dangerous,” noting that the AHA is actually making false claims since none of the four studies they included in their analysis involved coconut oil.
As an explanatory side note, most of the early studies on coconut oil that found less than favorable results used partially hydrogenated coconut oil, not unrefined virgin coconut oil.13 As always, the devil’s in the details, and hydrogenated oil is not the same as unrefined oil, even when you’re talking about something as healthy as coconut. This little detail is what led to the undeserved vilification of coconut oil in the first place. That said, let’s look at what else Shanahan has to say on the matter:
“Most doctors don’t notice that the medical leadership is making unfounded claims, and the reason they don’t notice is because … articles asserting the existence of human clinical trial evidence against coconut as well as all other foods high in saturated fat, conflate the sources of saturated fat with the saturated fat itself.
Saturated fat does not actually exist in the food chain; what they’re talking about are saturated fatty acids, the components of triglyceride fat, the substance chefs call simply ‘fat.’ We often say things like ‘coconut oil is a saturated fat’ and ‘butter is a saturated fat.’ But it would be more correct to say ‘coconut oil is high in saturated fatty acids.’
Coconut oil, butter, lard, tallow and every other animal fat also contain monounsaturated and even some polyunsaturated fatty acids in addition to saturated fatty acids … The idea is foods contain blends of fatty acids in varying proportion.”
Put another way, most foods contain a blend of fatty acids, not just one. Margarine and shortening also contain saturated fatty acids, yet the AHA makes no mention of this. The harder the margarine, the more saturated fat it tends to contain, in some cases more than butter or lard.
“So, when people eat margarine and shortening, in addition to toxic trans fatty acids they’re also eating saturated fatty acids. And that means that when a study says it’s swapping out saturated fat for vegetable oils, that does not equate to swapping out butter and lard. It could very well be the case that margarine and shortenings were among the foods that got eliminated,” Shanahan says.
“And because most doctors don’t realize that margarine and shortenings contain saturated fatty acids, they also don’t consider it particularly important to wonder whether or not studies like the four core citations mentioned in the Advisory are actually confounded by the fact that the baseline, high-saturated fat diet included a significant amount of margarines and shortenings that contain toxic trans fat.
Because if they did, then that means whatever health benefits were observed in the studies may have nothing to do with the reductions in saturated fat. It’s cutting back on trans fat that makes the difference to health.”
Anti-Saturated Fat Recommendations Have Been Followed With Disastrous Results
Since the 1950s, when vegetable oils began being promoted over saturated fats like butter, Americans have dutifully followed this advice, dramatically increasing consumption of vegetable oil. Soy oil, for example, has risen by 600 percent (10,000 percent from 1900) while butter, tallow and lard consumption has been halved. We’ve also dramatically increased sugar consumption.14
Alas, rather than becoming healthier than ever, Americans have only gotten fatter and sicker. Heart disease rates have not improved even though people have been eating what the AHA suggests is a heart-healthy diet. Common sense tells us if the AHA’s advice hasn’t worked in the last 65 years, it’s not likely to start working now.
As noted by Shanahan, technology that allows us to study molecular reactions is relatively recent, and certainly was not available back in the 60s and 70s. Modern research is just now starting to reveal what actually happens at the molecular level when you consume vegetable oil and margarine, and it’s not good. For example, Dr. Sanjoy Ghosh,15 a biologist at the University of British Columbia, has shown your mitochondria cannot easily use polyunsaturated fats for fuel due to the fats’ unique molecular structure.
Other researchers have shown the PUFA linoleic acid can cause cell death in addition to hindering mitochondrial function.16 PUFAs are also not readily stored in subcutaneous fat. Instead, the tends to get deposited in your liver, where they contribute to fatty liver disease, and in your arteries, where they contribute to atherosclerosis.
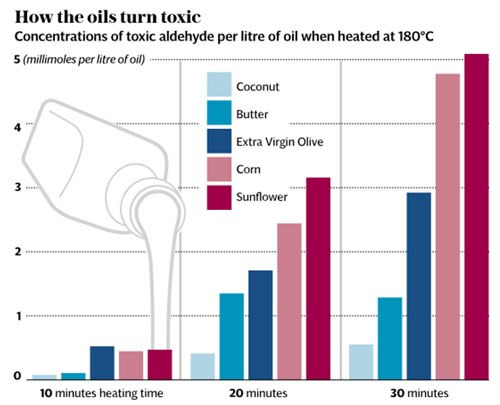
According to Frances Sladek,17 Ph.D., a toxicologist and professor of cell biology at UC Riverside, PUFAs behave like a toxin that builds up in tissues because your body cannot easily rid itself of it. When vegetable oils like sunflower oil and corn oil are heated, cancer-causing chemicals like aldehydes are also produced.18
Not surprisingly, fried foods are linked to an increased risk of death. Most recently, eating fried potatoes more than twice a week was found to double a person’s risk of death compared to never eating fried potatoes.19 Animal and human research has also found vegetable oils promote:
- Obesity and fatty liver20
- Lethargy and prediabetic symptoms21
- Chronic pain/idiopathic pain syndromes (meaning pain with no discernible cause)22
- Migraines23
- Crohn’s disease and ulcerative colitis24
Biochemistry Versus Statistics
According to Shanahan, the idea that PUFAs are healthier than saturated fats fall flat when you enter the field of biochemistry, because it’s “biochemically implausible.” In other words, the molecular structure of PUFA is such that it’s prone to react with oxygen, and these reactions disrupt cellular activity and cause inflammation.25 Oxidative stress and inflammation, in turn, are hallmarks not only of heart disease and heart attacks but of most chronic diseases.26,27
“Meanwhile, the folks at the AHA claim saturated fat is pro-inflammatory and causes arterial plaque and heart attacks — but there is no biochemically plausible explanation for their argument. Saturated fat is very stable, and will not react with oxygen the way PUFA fat does, not until the fundamental laws of the universe are altered,” Shanahan writes.
“Our bodies do need some PUFA fat, but we need it to come from food like walnuts and salmon or gently processed (as in cold pressed, unrefined) oils like flax and artisanal grapeseed, not from vegetable oils because these are refined, bleached and deodorized, and the PUFA fats are molecularly mangled into toxins our body cannot use.”
The Cholesterol Argument
Researchers have also laid waste to the notion that having high cholesterol is a primary contributor to heart disease in the first place. This is the basic premise upon which the AHA builds its conclusion that saturated fats are bad for you. The idea is that saturated fats raise your cholesterol level, thus raising your risk for heart disease. But again, they use too broad a brush and ignore the details. For example:
• A recent study28 published in The BMJ reanalyzed data from the Minnesota Coronary Experiment (MCE) that took place between 1968 and 1973, after gaining access to previously unpublished data. This was a double-blind, randomized controlled trial to test whether replacing saturated fat with vegetable oil (high in linoleic acid) would lower cholesterol levels, thus reducing heart disease and related deaths.
Interestingly, while the treatment group did significantly lower their cholesterol, no mortality benefit could be found. In fact, for each 30 milligrams per deciliter (mg/dL) reduction in serum cholesterol, the risk of death increased by 22 percent. Swapping saturated fat for vegetable oil also had no effect on atherosclerosis rates or heart attacks. As noted by the authors:
“Available evidence … shows that replacement of saturated fat in the diet with linoleic acid effectively lowers serum cholesterol but does not support the hypothesis that this translates to a lower risk of death from coronary heart disease or all causes. Findings … add to growing evidence that incomplete publication has contributed to overestimation of the benefits of replacing saturated fat with vegetable oils …”
• AHA also does not take LDL particle number into consideration. There are large, fluffy LDL particles and small, dense ones. We didn’t have this information in the 1960s, but we sure have it now.
This is yet another crucial detail that makes all the difference in the world, as large LDL particles have been shown to be harmless and do not raise your risk for heart disease. And guess what? Sugar promotes harmful small, dense LDLs while saturated fats found in butter and coconut oil promotes harmless large, fluffy LDLs29
Is Coconut Oil Healthy or Not?
The short answer is yes, coconut oil is healthy. It’s been a dietary staple for millennia, providing you with high-quality fat that is important for optimal health. It supports thyroid function, normalizes insulin and leptin function, boosts metabolism, and provides excellent and readily available fuel for your body in lieu of carbohydrates (which you need to avoid if you want to lose weight).
A really important benefit of coconut oil is related to the fact that the ketones your liver creates from it are the preferred fuel for your body, especially your heart and brain, and may be key for the prevention of heart disease and Alzheimer’s. It truly is a healthy staple that belongs in everyone’s kitchen.
Coconut oil contains medium chain triglycerides (MCTs), and their smaller particle size helps them penetrate your cell membranes more easily. However, MCT oil has a far higher concentration of these shorter chain fats that are more efficiently converted to ketones; C8 or caprylic acid has the best ability to convert to ketones.
MCTs do not require special enzymes and they can be utilized more effectively by your body, thus putting less strain on your digestive system. Normally, a fat taken into your body must be emulsified with bile from your gallbladder before it can be broken down and properly absorbed. Long chain fats therefore frequently end up being stored in your fat cells.
However, your body treats MCTs differently. MCTs bypass the bile and fat storage process and go directly to your liver, where they are converted into ketones. Your liver quickly releases the ketones into your bloodstream where they are transported around your body to be used as fuel. By being immediately converted into energy rather than being stored as fat, MCTs stimulate your body’s metabolism and help promote weight loss.
Coconut Oil Promotes Thyroid Health
Part of coconut oil’s health benefits also relate to its beneficial impact on your thyroid. Unlike many other oils, coconut oil does not interfere with T4 to T3 conversion, and T4 must be converted to T3 in order to create the enzymes needed to convert fats to energy.
Part of what makes processed vegetable oils so damaging to the thyroid is that they oxidize quickly and become rancid, which prevents the fatty acids from being deposited into your cells, thereby impairing the conversion of T4 to T3. This is symptomatic of hypothyroidism. Coconut oil is a saturated fat and therefore very stable and not susceptible to oxidation.
The fact that it doesn’t go rancid helps boost your thyroid function. Eliminating processed vegetable oils from your diet and replacing them with coconut oil can, over time, help rebuild cell membranes in your liver (where much of the thyroid hormone conversion occurs) and increase enzyme production. This will assist in promoting the conversion of T4 to T3 hormones.
The most common fat in coconut oil is lauric acid, often considered a “miracle” fat because of its unique health-promoting properties. Your body converts lauric acid into monolaurin, which has antiviral, antibacterial and antiprotozoal properties. Thyroid problems can often be traced back to chronic inflammation, which the lauric acid in coconut oil can help suppress. To obtain the full range of coconut oil’s health and weight loss benefits, I typically recommend 2 to 3 1/2 tablespoons per day for adults.
That said, there is at least one instance where coconut oil is contraindicated due to its lauric acid content. In his book, “The Plant Paradox: The Hidden Dangers in ‘Healthy’ Foods That Cause Disease and Weight Gain,” Dr. Steven Gundry explains how coconut oil may be problematic if you have leaky gut, which is almost universal in individuals who are not paying attention to their lectin intake.
As it turns out, lipopolysaccharide (LPS), an endotoxin, attaches to lauric acid, facilitating its transport past your gut lining into your blood stream. Interestingly, MCT oil does not do this. So, if you have leaky gut, or unless you’re healthy and eating a lectin free diet, it may be best to avoid coconut oil and use MCT oil instead. Caprylic acid would be best, but neither of these will allow LPS to piggyback into your blood stream. You can learn more about lectins in my interview with Gundry.
Who Pays the AHA?
Science has revealed the low-fat diet to be corporate-promoted misinformation, yet the AHA keeps insisting it’s the heart-healthy choice. Why? As noted by cardiologist Dr. Barbara Roberts in an article in The Daily Beast in 2014,30 “The quick answer: money, honey.” Roberts points out that one of the reasons the AHA clings to “recommendations that fly in the face of scientific evidence” is because of its ties to Big Food.
One of its primary revenue streams is its Heart Check Food Certification Program.31 Foods bearing this certification mark are supposed to make it easier for consumers to select products to include in a heart-healthy diet. Companies pay about $700,000 annually for the right to use this mark on their packaging.32 As of 2014, the AHA endorsed about 890 foods as heart-healthy, including breads, cereals, pastas and pasta sauces, potatoes, egg substitutes, dried and canned fruits and processed meats.33
In other words, a whole bunch of stuff you really shouldn’t eat if you care about your health in general and your heart in particular is on the list. Processed meats, for example, have been deemed so hazardous there’s no safe limit.34 The AHA also endorses Subway sandwiches35 and Cheerios,36 and is sponsored by a long list of drug companies.37 As noted by Roberts:38
“Even more problematic are the foods containing added sugar … The AHA recommends that women consume less than 6 teaspoons (100 calories) of sugar a day and less than 9 teaspoons (150 calories) for men.
Yet there are items that get the nod of approval from the Heart Check program despite being near or at the sugar limit, like Bruce’s Yams Candied Sweet Potatoes … Indeed, until 2010, the Heart Check imprimatur was stamped on a drink called Chocolate Moose Attack, which contained more sugar per ounce than regular Pepsi. And until [2014], Heart Check approved many foods with trans fats …”
AHA Was Wrong in the 1960s and Is Still Wrong
Heart disease is primarily caused by chronic inflammation, which is caused by excessive amounts of omega-6 (unbalanced omega-6 to omega-339), dangerous trans fats, processed vegetable oils and excessive sugar in the diet. Saturated fats, on the other hand, have been repeatedly exonerated, with studies showing they do not contribute to heart disease and are in fact a very important source of fuel for your body.
Granted, it’s tough to admit you’ve been wrong for 65-plus years. Such an admission can mar an organization’s reputation. But in trying to turn back the clock to 1960 and promote margarine and vegetable oils over butter and coconut oil, the AHA is proving itself obsolete.
This recommendation is, in my view, professionally irresponsible. It’s completely irrational in the face of modern nutritional science. With it, the AHA has painted itself into a corner from which it cannot extract itself without turning the entire organization upside-down. As noted by Dave Asprey, founder of Bulletproof.com,
“The AHA campaign is backfiring because of the millions of people who already know that adding undamaged saturated fats into their diets makes them feel better. They can feel the difference in their energy, see it in the mirror, and measure it in their blood work …
These anti-coconut oil AHA guidelines are an orchestrated PR campaign aimed at changing what we eat to match what is in the interests of the AHA’s corporate sponsors, regardless of what recent research suggests.
As the U.S. population gets more educated about the benefits of saturated fats and the harm posed by processed seed and vegetable oils, processed food manufacturers are looking for ways to trick us into eating the cheap, high profit, damaging ‘food’ they create and sell.
That appears to be why they sponsor the [AHA]. These new recommendations are from an industry special interest group that promotes low-fat, high-sugar diets that kill people and has the audacity to label them as ‘heart healthy.’ In fact, the AHA executive leading the charge against coconut oil is the same guy that used to run marketing for Kentucky Fried Chicken and other fast-food chains.”
Source:: Mercola Health Articles



 Body Charge Nutrition is a premium nutritional supplement provider based in Western Canada offering only products and information that are of the highest quality and integrity. Through knowledge and personal experience, it is our goal to assist you with taking control of your health.
Body Charge Nutrition is a premium nutritional supplement provider based in Western Canada offering only products and information that are of the highest quality and integrity. Through knowledge and personal experience, it is our goal to assist you with taking control of your health.